Platelet transfusion is an important supporting treatment for hematologic disorders, especially in bone marrow failure disease and post-chemotherapy myelosuppression. However, in patients experienced multiple transfusions, platelet transfusion refractoriness (PTR) occasionally happened. Up to date, many factors had been explored contribute to the PTR, including infections, splenomegaly, antibodies against human leukocyte antigen class I (HLA-I) and antibodies against human platelet antigens (HPA). Based on our clinical practice, we also discovered that many cases had experienced primary PTR (who have been experienced PTR since the first platelet transfusion). Those patients suffered from severe thrombocytopenia can only be effectively corrected by cross-matching platelet transfusion. To our knowledge, anti-HLA-I-A and B antibodies had been reported to be in reference to immune-mediated PTR, while there are no conclusions about primary PTR. Herein, we identified anti-HLA-C autoantibodies was an independent risk factor for the primary PTR in patients with hematologic disorders, even refractoriness to cross-matching platelet transfusion or HLA-selected platelet transfusion.
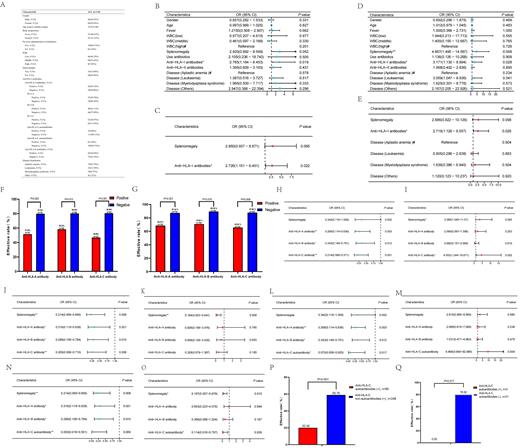
We retrospectively reviewed the patients that had HLA high resolution genotyping test report (potential for hematopoietic stem cell transplantation), and along with a donor-specific HLA antibodies (DSA) test or PRA testing potential for cross-matching platelet transfusion in our department between January 2019 and March 2023. 114 patients were enrolled, with a median age of 40 (14-80) years old, and the composition of disorders were aplastic anemia (65.8%), leukemia (21.9%), myelodysplastic syndrome (8.8%) and other (3.5%) (Fig A). Post-transfusion platelet efficacy was evaluated by the calculation of corrected count increment (CCI). The overall transfusion effective rate was 69.23% in this cohort, while 18.8% failed response from the first transfusion. Logistic regression analysis showed that only anti-HLA-I antibody contribute to the ineffectiveness of first and overall platelet transfusion (Fig B-E). In patients with positive anti-HLA-I antibodies, there were 35, 48 and 32 patients positive for anti-HLA-A, B and C antibodies, respectively (Fig A). Meanwhile, we surprisingly found that there were also 6 patients have anti-HLA-I autoantibody, including 6 on HLA-C and 1 have both HLA-A and C. To distinguish and gain a better understanding of the value of anti-HLA autoantibody in both TR and PTR, we further analyzed each locus of HLA-I and found that either anti-HLA-A, HLA-B or HLA-C antibody contribute to the ineffective to the overall and first platelet transfusion (Fig F-G), while logistic regression analysis revealed that only anti-HLA-C antibody was the independent risk factor (Fig H-K).
We performed a logistic regression analysis with factors of anti-HLA-A, B antibody and anti-HLA-C autoantibody, and results showed that the association between positive anti-HLA-C autoantibody and the occurrence of PTR was significant ( P=0.008) (Fig J-M), while a difference approached the significance was also observed in overall platelet transfusion analysis ( P=0.054) (Fig N-O). In detail, we found that the effective overall platelet transfusion in the 6 patients who had anti-HLA-C autoantibodies was 20% (18 out of 90 transfusion), while for patients only have anti-HLA-C non-autoantibodies, it was 59.76% (47 out of 246 transfusion), a significant difference was observed ( P<0.001) (Fig P). For 3 patients with positive anti-HLA-C autoantibodies, all experience ineffective cross-matching platelet transfusion; while for the patients whom without anti-HLA-C autoantibodies, 21 patients experience cross-matching platelet transfusion and 17 of them response quite well, whit a significantly differences ( P=0.017) (Fig Q).
In summary, our study demonstrated that positive anti-HLA-C autoantibody had a significant association with the occurrence of primary and overall PTR. The effects of cross-matching platelet transfusions in these patients are also unsatisfactory. To reduce the occurrence of PTR, our results suggested that it is necessary to anticipate the occurrence of PTR in patients with anti-HLA-C autoantibody positivity. Meanwhile, mechanisms should be explored and ways should be sought to lower the levels of such autoantibodies.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal